Brain Death Testing
One of the unfortunate situations that we deal with in the ICU is when patients progress to brain death. The most common causes that I have seen of brain death are from either a hemorrhagic stroke or a cardiac arrest which increased the patient's intracranial pressure causing herniation (the brain passing through the spinal column causing the most severe and irreversible brain damage).
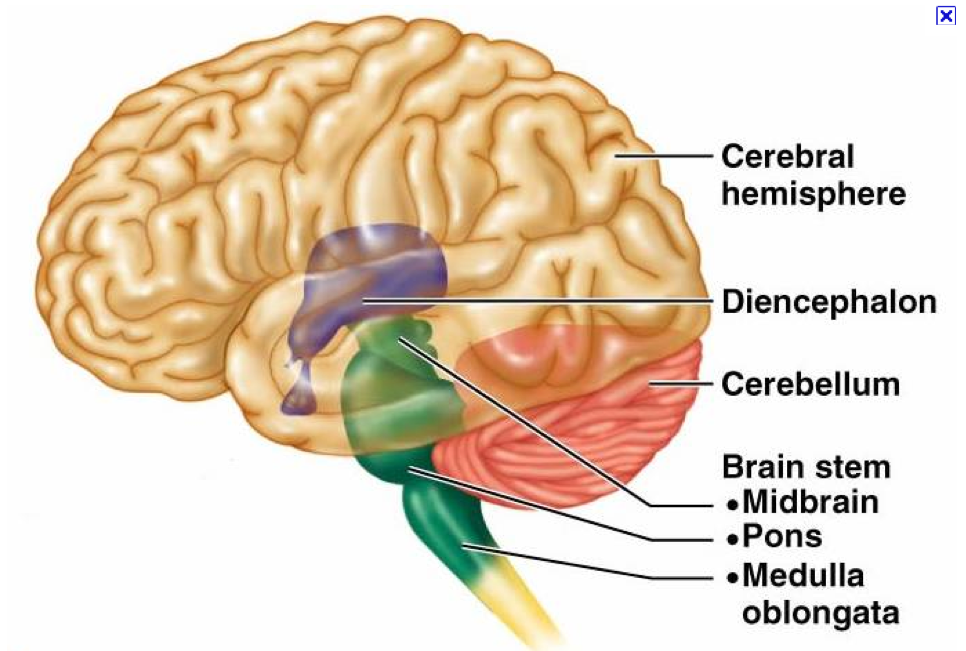
Different parts of the brain are responsible for different functions. The brainstem is made up of the midbrain, pons, and medulla oblongata.
Midbrain: responsible for vision, hearing, motor control, sleep/wake, arousal (alertness), and temperature regulation. With severe neurological damage, it is not uncommon to see extremely high, uncontrollable fevers.
Pons: regulates breathing and serves as a bridge or relay center for information transmitted between different parts of the brain. As herniation occurs, patients will lose all respiratory drive and not initiate any spontaneous breaths.
Medulla oblongata: deals with involuntary (autonomic) functions of the body including cardiac, respiratory, coughing, vomiting and vasomotor centers.
As the brain begins to herniate (pass through) through the foramen magnum, you see the functions of the brainstem begin to fail. Patients lose their pain response, the reflexes, and respiratory drive.
Brain death testing is very specific and is done by multiple doctors to confirm brain death. Oftentimes this testing is performed by intensivists or neurologists. The American Academy of Neurology has guidelines on establishing brain death as follows:
"Many of the details of the clinical neurologic examination to determine brain death cannot be established by evidence-based methods. The detailed brain death evaluation protocol that follows is intended as a useful tool for clinicians. It must be emphasized that this guidance is opinion-based. Alternative protocols may be equally informative.
The determination of brain death can be considered to consist of the following steps:
I. The clinical evaluation (prerequisites).
A. Establish irreversible and proximate cause of coma.
The cause of coma can usually be established by history, examination, neuroimaging, and
laboratory tests.
Exclude the presence of a CNS-depressant drug effect by history, drug screen, or, if available, drug plasma levels below the therapeutic range. Prior use of hypothermia (e.g., after cardiopulmonary resuscitation for cardiac arrest) may delay drug metabolism. The legal alcohol limit for driving (blood alcohol content 0.08%) is a practical threshold below which an examination to determine brain death could reasonably proceed.
There should be no recent administration or continued presence of neuromuscular blocking agents (this can be defined by the presence of a train of 4 twitches with maximal ulnar nerve stimulation).
There should be no severe electrolyte, acid-base, or endocrine disturbance. Achieve normal core temperature.
In most patients, a warming blanket is needed to raise the body temperature and maintain a normal or near-normal temperature (36°C).
B. Achieve normal systolic blood pressure.
Hypotension from loss of peripheral vascular tone or hypovolemia (diabetes insipidus) is common; vasopressors or vasopressin are often required. Neurologic examination is usually reliable with a systolic blood pressure 100 mm Hg.
C. Perform 2 neurologic examinations
Legally, all physicians are allowed to determine brain death in most US states. Neurologists, neurosurgeons, and intensive care specialists may have specialized expertise. It seems reasonable to require that all physicians making a determination of brain death be intimately familiar with brain death criteria and have demonstrated competence in this complex examination. Brain death statutes in the United States differ by state and institution. Some US state or hospital guidelines require the examiner to have certain expertise.
The clinical evaluation (neurologic assessment).
A. Coma.
Patients must lack all evidence of responsiveness. Eye opening or eye movement to noxious stimuli is absent. Noxious stimuli should not produce a motor response other than spinally mediated reflexes. The clinical differentiation of spinal responses from retained motor responses associated with
B. Absence of brainstem reflexes.
- Absence of pupillary response to a bright light is documented in both eyes.
- Absence of ocular movements using oculocephalic testing and oculovestibular reflex testing. Movement of the eyes should be absent during 1 minute of observation. Both sides are tested, with an interval of several minutes.
- Absence of corneal reflex. Absent corneal reflex is demonstrated by touching the cornea with a piece of tissue paper, a cotton swab, or squirts of water. No eyelid movement should be seen.
- Absence of facial muscle movement to anoxious stimulus.
- Absence of the pharyngeal and tracheal reflexes. The pharyngeal or gag reflex is tested after stimulation of the posterior pharynx with a tongue blade or suction device. The tracheal reflex is most reliably tested by examining the cough response to tracheal suctioning. The catheter should be inserted into the trachea and advanced to the level of the carina followed by 1 or 2 suctioning passes.
C. Apnea Test
- Absence of a Respiratory Drive.
Absence of a breathing drive is tested with a CO2 challenge. Documentation of an increase in PaCO2 above normal levels is typical practice. It requires preparation before the test.
Prerequisites:
- normotension
- normothermia
- euvolemia
- eucapnia (PaCO2 35–45 mm Hg)
- absence of hypoxia
- no prior evidence of CO2 retention (i.e., chronic obstructive pulmonary disease, severe obesity).
Procedure:
- Adjust vasopressors to a systolic blood pressure _100 mm Hg.
- Preoxygenate for at least 10 minutes with 100% oxygen to a PaO2 _200 mm Hg.
- Reduce ventilation frequency to 10 breaths per minute to eucapnia.
- Reduce positive end-expiratory pressure (PEEP) to 5 cm H2O (oxygen desaturation with decreasing PEEP may suggest difficulty with apnea testing).
- If pulse oximetry oxygen saturation remains_95%, obtain a baseline blood gas (PaO2, PaCO2, pH, bicarbonate, base excess).
- Disconnect the patient from the ventilator.
- Preserve oxygenation (e.g., place an insufflations catheter through the endotracheal tube and close to the level of the carina and deliver 100% O2 at 6 L/min).
- Look closely for respiratory movements for 8–10 minutes. Respiration is defined as abdominal or chest excursions and may include a brief gasp.
- Abort if systolic blood pressure decreases to _90 mm Hg.
- Abort if oxygen saturation measured by pulse oximetry is _85% for _30 seconds. Retry procedure with T-piece, CPAP 10 cm H2O, and 100% O2 12 L/min.
- If no respiratory drive is observed, repeat blood gas (PaO2, PaCO2, pH, bicarbonate, base excess) after approximately 8 minutes.
- If respiratory movements are absent and arterial PCO2 is _60 mm Hg (or 20 mm Hg increase in arterial PCO2 over a baseline normal arterial PCO2), the apnea test result is positive(i.e., spports the clinical diagnosis of brain death).
If the test is inconclusive but the patient is hemodynamically stable during the procedure, it may be repeated for a longer period of time (10–15 minutes) after the patient is again adequately pre-oxygenated.
Ancillary tests
In clinical practice, EEG, cerebral angiography, nuclear scan, TCD, CTA, andMRI/MRA are currently used ancillary tests in adults (see below).
Common Confirmatory Tests In Brain Death
Cerebral angiography
- Contrast medium under high pressure in both anterior and posterior circulation injections
- No intracerebral filling at the level of the carotid or vertebral artery entry to the skull
- Patent external carotid circulation
- Possible delayed filling of the superior longitudinal sinus
Electroencephalography
- Minimum of eight scalp electrodes
- Interelectrode dependencies should be between 100 and 10,000
- Integrity of the entire recording system should be tested
- Electrode distances should be at least 10 cm
Sensitivity should be increased to at least 2 µV for 30 minutes with inclusion of appropriate calibrations - High-frequency filter setting should be at 30 Hz, and low-frequency setting should not be below 1 Hz
- There should be no electroencephalographic reactivity to intense somatosensory or audiovisual stimuli
Transcranial Doppler ultrasonography
- Bilateral insonation.
- The probe is placed at the temporal bone above the zygomatic arch or the vertebrobasilar arteries through the suboccipital transcranial window•
- The abnormalities should include a lack of diastolic or reverberating flow, small systolic peaks in early systole, and a lack of flow found by the investigator who previously demonstrated normal velocities
Cerebral scintigraphy (technetium Tc 99m hexametazime)
- Injection of isotope within 30 minutes of reconstitution
- Static image of 500,000 counts at several time intervals: immediately, between 30 and 60 minutes, and at 2 hours.
Information based on: Evidence-based guideline update: Determining brain death in adults: Report of the Quality Standards Subcommittee of the American Academy of Neurology Eelco F.M. Wijdicks, Panayiotis N. Varelas, Gary S. Gronseth and David M. Greer 181e242a8 Neurology 2010;74;1911-1918"
After establishing that a patient is brain dead, oftentimes donor services will get involved to see what the patient's wishes were regarding organ donation. This is a very sensitive topic that is addressed delicately with the family. If they agree to organ donation, the treatment of this patient is very labor intensive as the nurses manage all of the patient's body systems to maintain healthy organs for donor recipients.